Prescription Medication and Substance Abuse
If you’re taking prescription medications for a mental health disorder along with using recreational drugs or alcohol, the interaction could lead to dangerous health consequences. Read ahead to learn why mental illness often coexists with drug addiction, and about the risks attached to prescription medication and substance abuse.
Mental Illness and Substance Abuse Often Occur Together
When a person is diagnosed with two or more disorders, that phenomenon is defined as comorbidity. Comorbidity of mental illness and substance abuse disorder is fairly common, and many studies have found that close to 50 percent of those who suffer from a mental health disorder will also experience problems with substance abuse.[7] The reverse is also true: a substance abuse problem may lead to a future diagnosis of a mental health disorder.[7]
Comorbidity is also known as co-occurring disorders and dual diagnosis. Dual diagnosis indicates only that the two disorders exist. It doesn’t mean they necessarily happen at the same time or that one disorder causes the other. While we can’t unravel the mystery of causation, we do know which factors can contribute to the comorbidity of mental illness and a substance use disorder.
Risk Factors That Can Contribute to Both Mental Illness and Substance Abuse
Genetic Factors
Several studies have found a link between substance abuse and genetics. For example, if a family member is addicted to alcohol, there’s a 40-60 percent chance someone who shares his genes will inherit the disease[1], and genetics may determine is someone is predisposed to be a heavy user of marijuana and other illicit drugs[2]. But research also indicates that there are genes that could contribute to both addiction and mental disorders[3].
Brain Chemistry
Substance abuse and mental illness are both capable of affecting or disrupting many areas of the brain – particularly those involved with reward systems, impulse control, and decision-making[4]. Additionally, both mental illness and illicit drug use can affect the neurotransmitters responsible for the release of dopamine, GABA, glutamate, norepinephrine, and serotonin[5].
Environmental Factors
Environmental factors like stress and childhood trauma can play a role in both the onset of mental illness and the likelihood of becoming addicted to drugs or alcohol. A 2010 study[6] found that there was a greater risk of developing a substance abuse problem among bipolar patients who reported being physically abused during childhood. A separate study found children who experienced trauma were more likely to be later diagnosed with PTSD as well as have a greater dependence on drugs like alcohol, marijuana, and cocaine[7].
Mental Disorders and their Contribution to Substance Abuse
In addition to the above risk factors for developing mental illness and substance abuse comorbidity, researchers have found that mental illness itself can be a contributing factor to drug addiction. If individuals who suffer from mental illness use street drugs or alcohol to self-medicate, they may be able to temporarily relieve their symptoms.
But brain anomalies due to the specific mental disorder may make it more likely to become addicted to the illicit drugs taken for temporary relief[7]. In other words, brain activity may make it more likely for the individual to experience enhanced results when taking street drugs or alcohol and to ignore any of the negative effects.
Substance Abuse Can Contribute to the Development of Mental Disorders
Neurotransmitters that are disrupted in patients with anxiety, depression, and bipolar disorder can also be affected by substance abuse. Additionally, it’s possible for drug use to trigger – via changes in brain structure – an underlying predisposition to a specific mental illness[5].
Continued after infographic:
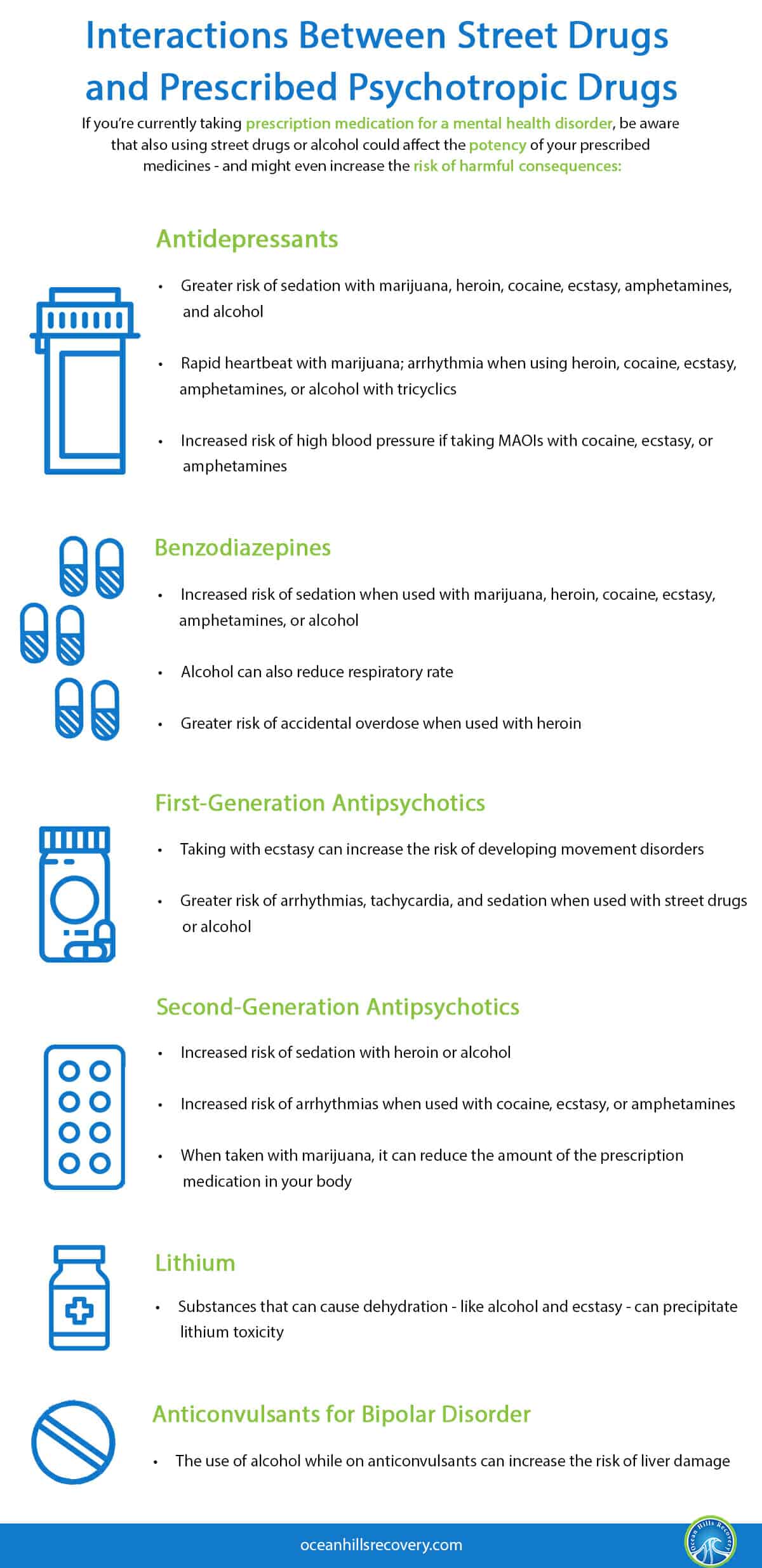
Interactions Between Street Drugs and Prescribed Psychotropic Drugs
If you’re currently taking prescription medication for a mental health disorder, be aware that also using street drugs or alcohol could affect the potency of your prescribed medicines – and might even increase the risk of harmful consequences:
Prescribed Drug |
Interaction With Recreational Drugs or Alcohol |
| Antidepressants |
|
| Benzodiazepines |
|
| First-Generation Antipsychotics |
|
| Second-Generation Antipsychotics |
|
| Lithium |
|
| Anticonvulsants for Bipolar Disorder |
|
Source: [8]
Prescription Medication and Substance Abuse: Where to Seek Treatment
The Dual Diagnosis program at Ocean Hills Recovery can provide help for those who struggle with both a mental health disorder and a substance abuse problem. Treatment for addiction alone can likely be unsuccessful if underlying mental illness isn’t addressed.
The approach to dual diagnosis at Ocean Hills Recovery is different from more traditional methods for treating addiction. Our “Collaborative Recovery” process involves therapists, physicians, family members, and the community to better understand an individual’s disorders and addictions. By combining medical, psychological, social, and spiritual interventions, we’re working to provide the greatest possibility of enduring recovery.
Find Out More About Dual Diagnosis Treatment
If you’re ready for a better approach to addiction treatment, contact Ocean Hills Recovery For more information about our Dual Diagnosis program. Long-term recovery is in your future!
Sources:
[1] https://pubmed.ncbi.nlm.nih.gov/19062348/
[2] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2879628/
[3]https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2888715/
[4]https://pubmed.ncbi.nlm.nih.gov/22986797/
[6] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2924768/
[7] https://pubmed.ncbi.nlm.nih.gov/21049532/
[8]http://oxleas.nhs.uk/site-media/cms-downloads/Street.Drugs.2688.pdf